Overview of components
The integration of Osigu Claims between a payer and multiple providers involves various systems, applications, and APIs. These components work together to streamline the authorization process and ensure seamless stakeholder interaction.
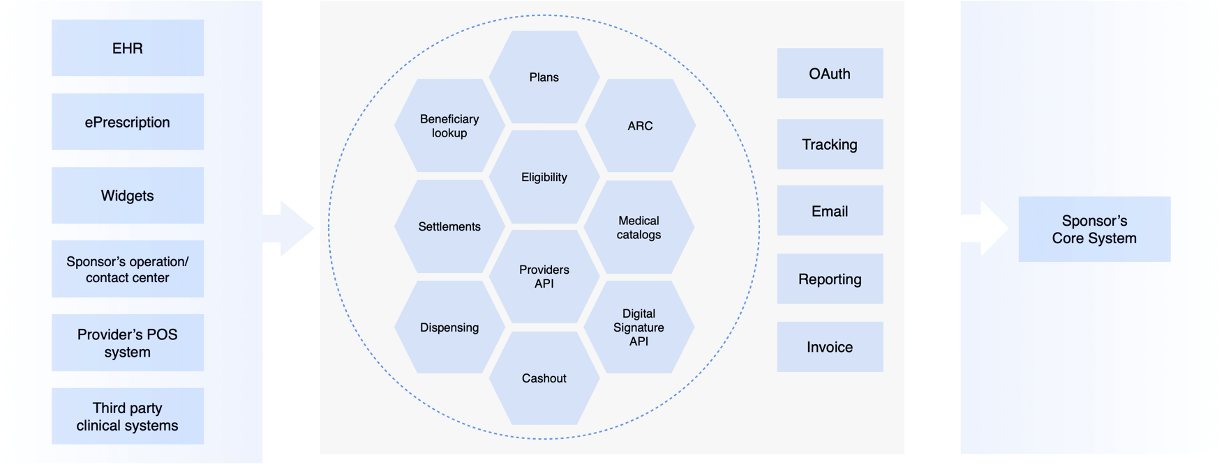
Participants in the Claims Integration
Authorizations and pre-authorizations can originate from various sources, whether through API integrations or Osigu’s applications. These include:
-
HIS or Electronic Health Record Systems:
- Clinics and hospitals use them to generate pre-authorizations and authorization claims.
-
Osigu eRX:
- Comprising an ambulatory EHR and a prescription web platform, eRX allows healthcare providers to create pre-authorizations (prior authorizations) directly.
-
Pre-Authorization Widget:
- A third-party JavaScript widget that builds a complete UI on the host site. It integrates with Osigu’s APIs to generate authorizations seamlessly.
-
POS Systems:
- Labs, diagnostic centers, and pharmacy chains use them. These systems integrate with Osigu’s APIs to create pre-authorizations and claims.
-
Payer Systems:
- Payers can generate authorizations and pre-authorizations directly from their internal systems.
-
Osigu Provider Web Portal:
- This portal, aimed at providers, allows quick onboarding without requiring immediate API integration. Providers can manage pre-authorizations and view transaction history.
-
Osigu Authorization Web Portal:
- Aimed at payers, this portal offers insights into operations and transaction management within Claims.
-
Payer Systems for Data Management:
- These systems feed the platform with the policyholder and beneficiary information while receiving notifications from Osigu.
Core Osigu Components
The following Osigu components power the Claims platform, handling data processing, validations, and integration:
-
Beneficiary Lookup API:
- Handles beneficiary and dependent searches using various search forms configured based on payer requirements.
-
ARC API:
- Manages transaction registration for authorizations, claims, and reimbursements.
- Provides controls such as medication waste minimization, pricing agreements between payers and providers, and fraud prevention rules.
-
Eligibility API:
- Validates data during pre-authorization (prior authorization) or authorization requests.
- Checks against policy conditions, including beneficiary coverage, exclusions, and medical protocols.
-
Plans API:
- Manages policies, groups, beneficiaries, coverages, exclusions, and pre-existing conditions.
- Tracks maximum coverage balances based on registered transactions or updates made by the payer.
-
Medical Catalogs API:
- Provides standard medical catalogs used across the healthcare industry.
- Supports platform operations and is available for clients to enhance their processes.
-
Auth Server:
- Osigu’s OAuth 2.0-based authentication and authorization server ensures secure access to all platform components.
The integration of Osigu Claims relies on these systems and APIs to deliver a unified, efficient, and reliable platform. By combining diverse sources of authorization requests with robust backend processing and validation components, Osigu ensures seamless operations for payers and providers, empowering healthcare stakeholders with streamlined workflows and transparent processes.
Updated 9 months ago
